Introduction to the FLACC Pain Scale
Origins and Development of the FLACC Scale
The FLACC pain scale, an acronym for Face, Legs, Activity, Cry, and Consolability, was developed in 1997 by Sandra Merkel, Patricia Voepel-Lewis, and Terri Shay at the University of Michigan Health System. This behavioral pain assessment tool was designed to address the need for a reliable and valid method to measure pain in children and non-verbal patients. Since its inception, the FLACC scale has become a widely-accepted standard in pediatric and adult care settings for pain assessment.
Purpose of the FLACC Pain Scale
The primary goal of the FLACC pain scale is to provide healthcare professionals with a comprehensive, yet easy-to-use tool for assessing pain levels in patients who cannot communicate their pain verbally. This includes young children, patients with cognitive impairments, and those under sedation or experiencing severe pain. By allowing healthcare providers to objectively assess pain levels in these vulnerable populations, the FLACC scale promotes accurate pain management and improved patient outcomes.
Comparison to Other Pain Scales
While numerous pain assessment tools exist, the FLACC pain scale stands out due to its focus on behavioral observation. Other common scales, such as the Numeric Rating Scale (NRS) and the Visual Analog Scale (VAS), rely heavily on patient self-reporting, which may not be feasible in certain populations. The FLACC scale provides a valuable alternative for healthcare professionals, offering a comprehensive framework for assessing pain through objective observation of patient behaviors.

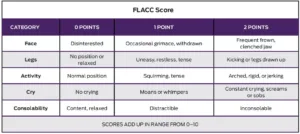
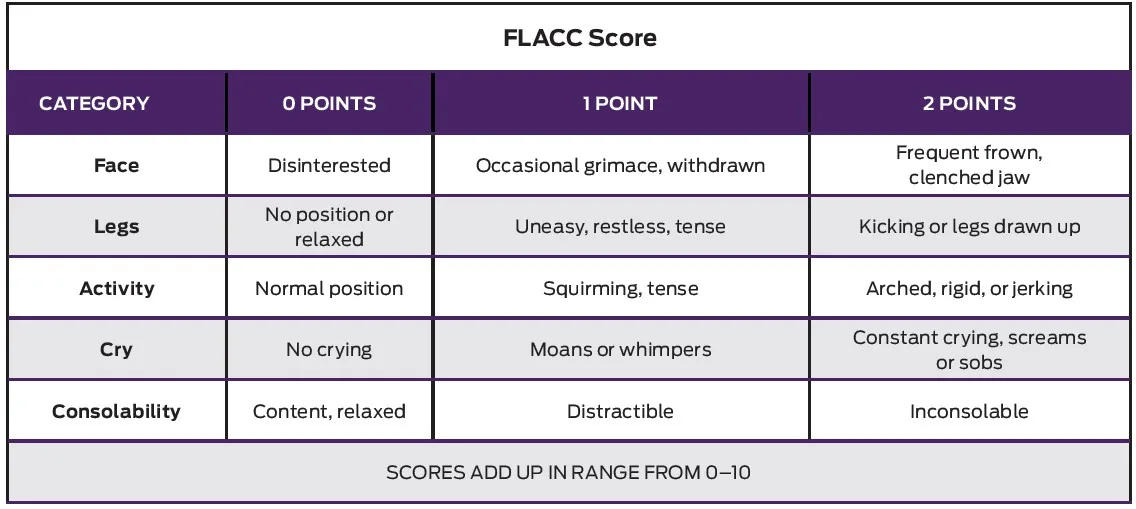
Components of the FLACC Pain Scale
Face (F)
The first component of the FLACC scale evaluates the patient’s facial expression. Healthcare providers assess the patient’s face for signs of discomfort, such as grimacing, clenched jaw, furrowed brow, or tightened facial muscles. A relaxed and neutral facial expression typically indicates low pain levels, while a tense or distorted face may suggest higher pain levels.
Legs (L)
The second component of the scale examines the patient’s legs. Providers look for signs of restlessness, such as kicking, squirming, or tense leg muscles. They also observe whether the patient’s legs are relaxed, bent, or drawn up toward the body, as these positions may indicate varying degrees of pain.
Activity (A)
The activity component assesses the patient’s overall body movement. Providers observe if the patient is lying still, squirming, or actively resisting movement. Increased agitation or resistance to movement can be indicative of higher pain levels, while a calm and relaxed demeanor suggests lower pain levels.
Cry (C)
The cry component focuses on the patient’s vocalizations. Healthcare providers listen for moaning, whining, or crying, and consider the intensity and frequency of these sounds. A quiet or content patient typically indicates lower pain levels, while a patient with frequent or intense vocalizations may be experiencing more severe pain.
Consolability (C)
The final component evaluates the patient’s ability to be consoled or comforted. Providers assess whether the patient can be easily calmed or soothed through comforting actions, such as holding, rocking, or verbal reassurance. A patient who can be easily consoled may have lower pain levels, while one who remains inconsolable despite attempts at comfort may be experiencing more intense pain.
Using the FLACC Pain Scale in Practice
Assessing Pain in Children and Non-Verbal Patients
When using the FLACC pain scale, healthcare providers systematically observe patients’ behaviors based on the five components mentioned earlier. It is crucial to conduct this assessment in a quiet, non-distracting environment to ensure accurate observations. Providers should spend adequate time observing each component and, if possible, compare their findings with baseline behaviors to determine any changes. In pediatric settings, involving parents or caregivers in the assessment process can be beneficial, as they are often familiar with the child’s typical behavior and reactions to pain.
Interpreting the FLACC Scores
The FLACC pain scale uses a scoring system that ranges from 0 to 10, with 0 representing no pain and 10 representing severe pain. Each of the five components is scored from 0 to 2, and the total score is calculated by summing the individual component scores. Generally, scores of 0-3 indicate mild pain, 4-6 suggest moderate pain, and 7-10 signify severe pain. Providers should use these scores as a guide for evaluating patients’ pain levels and adjusting their treatment plans accordingly.
Adjusting Treatment Based on FLACC Scores
Healthcare providers should use the FLACC pain scale scores to guide their treatment decisions, including pain management interventions and medication adjustments. For patients with mild pain, non-pharmacological interventions, such as distraction techniques, relaxation exercises, or cold/warm therapy, may be sufficient. Moderate pain may require additional interventions, such as the administration of analgesics or nonsteroidal anti-inflammatory drugs (NSAIDs). In cases of severe pain, stronger pain relief medications, such as opioids, may be necessary. Providers should continually reassess patients’ pain levels using the FLACC scale and adjust their treatment plans as needed to ensure effective pain management.

Benefits and Limitations of the FLACC Pain Scale
Advantages of Using the FLACC Scale
The FLACC pain scale offers several benefits for healthcare providers, particularly when assessing pain in children and non-verbal patients. First, its reliance on objective behavioral observations makes it suitable for patients who cannot self-report their pain levels. Second, the FLACC scale is easy to learn and use, allowing for quick and efficient pain assessments. Third, its comprehensive approach promotes accurate pain management and improved patient outcomes by considering multiple aspects of the patient’s behavior.
Challenges and Potential Drawbacks
Despite its many advantages, the FLACC pain scale also has some limitations. One potential drawback is that the scale’s reliance on behavioral observation may lead to subjective interpretations, especially if healthcare providers have different perspectives on what constitutes a specific behavior. Additionally, certain conditions, such as autism or other developmental disabilities, may present atypical pain behaviors that are not adequately captured by the FLACC scale. Furthermore, the FLACC scale may not always be appropriate for assessing pain in older children and adolescents who can communicate their pain levels more effectively through self-reporting. Healthcare providers should consider these limitations when using the FLACC scale and, if necessary, supplement their assessments with other pain measurement tools to ensure accurate and comprehensive pain management.
Improving Pain Management with the FLACC Scale
Role of FLACC in a Comprehensive Pain Assessment
The FLACC pain scale plays a crucial role in providing a comprehensive pain assessment, particularly for children and non-verbal patients. By incorporating the FLACC scale into routine care, healthcare providers can objectively measure pain levels and adjust treatment plans accordingly. However, it is essential to recognize that the FLACC scale should not be used in isolation. Providers should consider additional factors, such as patient history, clinical signs, and other assessment tools, to ensure a thorough understanding of the patient’s pain experience and appropriate management.
Collaboration Between Healthcare Professionals
Effective pain management requires collaboration between various healthcare professionals, including physicians, nurses, pharmacists, and therapists. By working together and consistently using the FLACC scale, healthcare teams can ensure that pain is accurately assessed and properly managed. Regular communication among team members is crucial for sharing insights, discussing treatment adjustments, and maintaining continuity of care.
Continuing Education and Training on Pain Assessment
To optimize the use of the FLACC pain scale and enhance pain management, healthcare providers should participate in ongoing education and training on pain assessment. This includes learning about the latest research, best practices, and emerging tools for measuring pain. Training should emphasize the importance of consistent and accurate use of the FLACC scale, as well as the need for clear communication among team members. By staying up-to-date on pain assessment techniques, providers can ensure that their patients receive the highest quality care and achieve better outcomes.
Conclusion: The Importance of Accurate Pain Assessment
Impact of Proper Pain Management on Patient Outcomes
Accurate pain assessment is essential for providing effective pain management and improving patient outcomes. By using tools like the FLACC pain scale, healthcare providers can more precisely gauge pain levels in vulnerable populations and tailor treatment plans accordingly. Proper pain management can lead to reduced hospital stays, faster recovery, improved patient satisfaction, and an overall better quality of life for patients.
Future Developments in Pain Assessment Tools
As our understanding of pain and its management continues to evolve, so will the tools and techniques used to assess it. Future developments in pain assessment may include innovations in technology, such as wearable devices or advanced imaging, as well as the integration of artificial intelligence and machine learning to enhance the accuracy and efficiency of pain measurement. Additionally, research into pain assessment in specific populations, such as those with cognitive impairments or unique cultural backgrounds, will help refine existing tools and develop new methods to better serve all patients. By embracing these advancements, healthcare providers can continue to improve pain management and ensure the highest standard of care for their patients.
See All Posta Related Pain Assessment
Revised FLACC Tool: Reliable Pain Assessment for Children with Cognitive Impairment
New Study Evaluates Pain Assessment Tools for Infants and Young Children